For many years the EmergiQuiz presentations have been one of the highlights of the AAP National Conference and Exhibition Section on Emergency Medicine Program. Pediatric Emergency Medicine Fellows present challenging cases and another fellow attempts to make the diagnosis. This is followed by an educational presentation that focuses not just on the rare diagnosis, but also the general learning inherent to the case. This post highlights a recent EmergiQuiz case.
The original EmergiQuiz case, entitled “Extremity Fractures in an Infant” was submitted by Rachel Cafferty, MD and Michelle Alletag, MD from Colorado Children’s
Objectives
- Appreciate that syphilis rates are rising in the United States.
- Recognize clinical features of early congenital syphilis and late congenital syphilis.
- Understand the diagnostic workup and radiographic findings unique to congenital syphilis.
- Review treatment for congenital syphilis and the most common complication associated with treatment.
Over the past decade, national trends have demonstrated increased rates of primary and secondary syphilis in the United States, particularly in western states.1
Syphilis is caused by the spirochete Treponema pallidum, which is usually sexually transmitted but can be spread by vertical transmission, trans-placentally from an infected mother to her unborn fetus at any stage of pregnancy, resulting in congenital syphilis in infants. Antenatal treatment with a single dose of penicillin G is >98% effective at preventing congenital syphilis.2 About 40% of pregnancies in women with untreated syphilis end in perinatal death,3 highlighting the importance of prenatal testing and maternal treatment. Rising rates of adult syphilis with poor prenatal care and low treatment rates, have resulted in a recent rise in cases of congenital syphilis.4 In 2017, the number of cases of congenital syphilis was the highest it had been in 20 years.5
Pediatric Emergency Medicine physicians must recognize the signs of congenital syphilis to make a timely diagnosis and initiate early treatment to decrease the sequelae of this infection.
Clinical manifestations of earlycongenital syphilis typically present between 3 weeks and 3 months of age, but can manifest at any point before two years of age. Infants may develop syphilitic rhinitis (the “snuffles”) as early as the first week of life. Syphilitic rhinitis is more severe than classic rhinitis associated with the common cold. Approximately 1-2 weeks after onset of rhinitis, a nonspecific red/pink rash develops which may progress to a copper/brown color with or without desquamation or scaling, involving the palms and soles, buttock and thighs. Syphilis is one of a handful of infections with a characteristic rash distribution involving the palms and soles. Both syphilitic rhinitis and cutaneous lesions contain spirochetes and are highly contagious through direct contact exposures. Bony abnormalities, most commonly diffuse periostitis and osteopenia are a common finding in congenital syphilis, resulting in pain for the affected infant. Pseudoparalysis of parrot (lack of movement of an extremity secondary to pain from bony lesions) is less common but pathognomonic for the disease. Pseudoparalysis of parrot more commonly involves upper extremities, is usually unilateral, and is poorly correlated with radiographic abnormalities. Other early findings in congenital syphilis include lymphadenopathy, hepatosplenomegaly, and jaundice.6
Late congenital syphilis is characterized by the Hutchinson’s triad which includes:
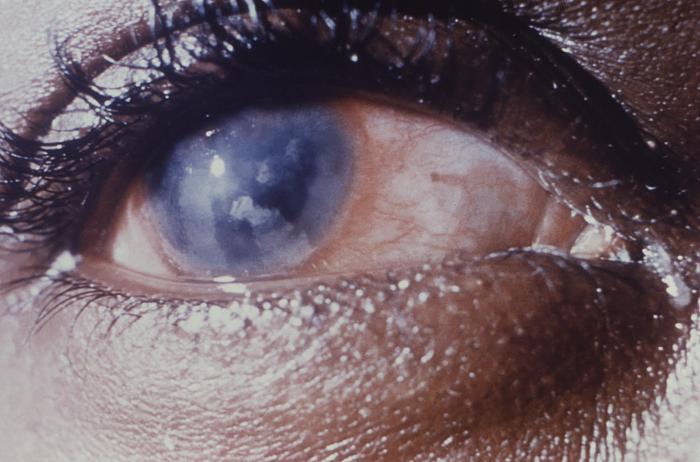
- Interstitial keratitis
- Sensorineural hearing loss (cranial nerve 8 deafness)
- Hutchinson teeth (blunted upper incisors)
Interstitial keratitis involves bilateral corneal scarring and secondary glaucoma, resulting in blindness that often manifests around puberty. Sensorineural hearing loss is most common between age 8-10 years, with loss of high frequency sound occurring first. In addition to Hutchinson teeth, patients may have mulberry molars or perforation of the hard palate (which is virtually pathognomonic for congenital syphilis). Characteristic facial features of late congenital syphilis include frontal bossing and saddle nose deformity. Skeletal deformities, such as anterior bowing of the shins (saber shins) are also commonly seen.6
The classic radiographic finding in congenital syphilis is periostitis (irregular periosteal thickening) that is symmetric and bilateral and typically involves multiple long bones. This may be mistaken as non-accidental trauma (NAT) and must be carefully distinguished by healthcare providers. Other radiographic findings of congenital syphilis include Wegner sign (metaphyseal serration or “sawtooth metaphysis”) and Wimberger sign (demineralization and osseous destruction of the upper medial tibia). The bony lesions described above are considered pathognomonic for congenital syphilis.7, 8There is no callus formation to suggest healing fractures, which further helps delineate radiographic findings from NAT.
Laboratory workup for congenital syphilis includes serum rapid plasma regain (RPR) and serum fluorescent treponemal antibody absorption (FTA-ABS) testing as well as cerebral spinal fluid (CSF) testing for venereal disease research laboratory (VDRL). Reactive CSF VDRL indicates neurosyphilis. Congenital syphilis is treated with a 10-day course of IV penicillin G, with a longer duration of treatment indicated in cases of neurosyphilis (14-day treatment course).
The Jarisch-Herxheimer reaction is observed in 50% of patients with primary syphilis and about 90% of patients with secondary syphilis.9The reaction is associated with initiation of antimicrobial treatment, which results in lysis of bacterial cell membranes and release of bacterial toxins into the bloodstream creating a systemic inflammatory response. While the reaction is usually not life-threatening and self-limiting, it may resemble bacterial sepsis. Patients may develop fever, chills, rigors, tachycardia, hypotension, hyperventilation, flushing of skin, myalgias, and exacerbation of skin lesions. Treatment is often supportive, and primarily involves use of antipyretics.
Rates of congenital syphilis are increasing in the United States, and what was once considered a rare diagnosis in pediatrics is becoming more commonly encountered in practice. Pediatric Emergency Medicine providers should consider congenital syphilis in any infant or young child with symptoms or diagnostic studies as listed above, and initiate treatment early in the hopes of best preventing against lifelong sequelae of this disease.
References
- Centers for Disease Control and Prevention (2018, July 24). Syphilis. Sexually Transmitted Disease Surveillance 2017. Retrieved from https://www.cdc.gov/std/stats17/syphilis.htm
- Alexander JM, Sheffield JS, Sanchez PJ, et al. Efficacy of treatment for syphilis in pregnancy. Obstetrics and Gynecology.1999;93(1):5-8
- Finelli L, Berman SM, Koumans EH, et al. Congenital syphilis. Bulletin of the World Health Organization.1998;76(2):126-128
- Bowen V, Su J, Torrone E, et al. Increase in Incidence of Congenital Syphilis – United States, 2012-2014. MMWR Morbidity and Mortality Weekly Report 2015;64(44):1241-1245
- Centers for Disease Control and Prevention (2018, September 25). Newborn syphilis cases more than double in four years, reaching 20-year high. CDC Newsroom. Retrieved from https://www.cdc.gov/media/releases/2018/p0925-newborn-syphilis-cases.html
- Dobson SR. Congenital syphilis: Clinical features and diagnosis. (2019) In C. Armsby (Ed.), UpToDate. Retrieved October 3, 2019, from UpToDate
- Sachdev M, Bery K, Chawla S. Osseous manifestations in congenital syphilis: A study of 55 cases. Clinical Radiology.1982;33:319-323
- Rasool MN, Govender S. The skeletal manifestations of congenital syphilis: A review of 197 cases.Journal of Bone and Joint Surgery British Volume.1989;71(5):752-755
- Lukehart, Sheila A. (2017). “Syphilis”. In Kasper, Dennis L.; Fauci, Anthony S. (eds.). Harrison’s Infectious Diseases (3 ed.). New York: Mc Graw-Hill. p. 666.












