It is possible for an adolescent to have a myocardial infarction. Maybe they had a previous history of Kawasaki Disease – or they have myocarditis, or a lipid metabolism disorder. It is also true that you are much more likely to see “benign early repolarization” on an EKG in a teenager (or young-ish adult up to age 50). Early Repolarization is widespread ST segment elevation that is also known as “J-point elevation” that looks like MI or myocarditis. Per Life in the Fast Lane, the features of benign early repolarization are:
- Widespread concave ST elevation, most prominent in the mid-to-left precordial leads (V2-5)
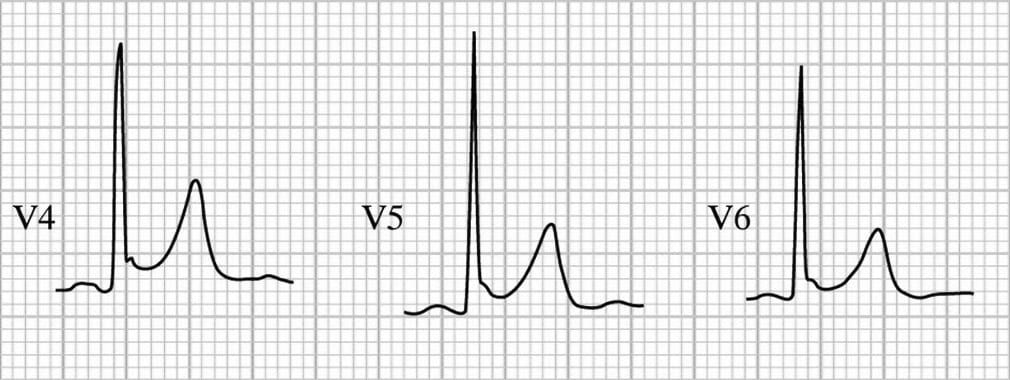
- Notching or slurring at the J point (best seen in V4)
- Prominent, slightly asymmetrical T waves that are concordant with the QRS complex
- ST elevation : T wave height ratio in V6 < 0.25 (see below)
- No reciprocal ST depression to suggest Occlusion MI
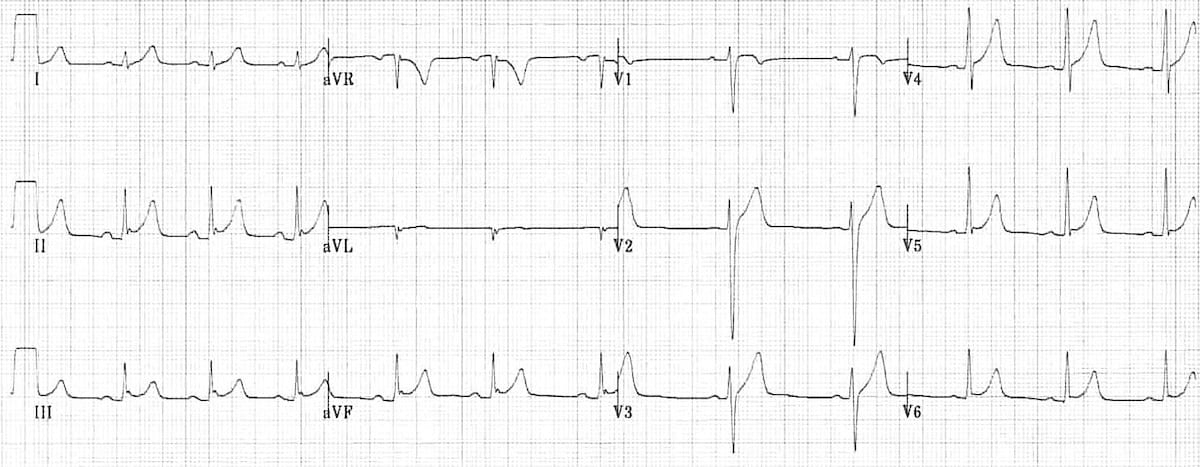
The above EKG shows Benign Early Repolarization. See if you can pick out the following characteristics:
- Generalised concave ST elevation in precordial (V2-6) and limb leads (I, II, III, aVF)
- J-point notching is evident in the inferior leads (II, III and aVF)
- ST elevation : T wave ratio < 0.25 in V6
Here are some examples of the J-point notching (the “fish hook”) of benign early repolarization in precordial leads – note that the notching is best seen in V4:
OK – so I know what you’re feeling right now if you’re reading this and you are Pediatric Emergency Medicine or General Pediatrics. Shoot! I kinda need to look at some STEMI EKGs to remember what they look like because I feel bad that I don’t know enough about what they actually look like… Go ahead, here’s a great link.
Welcome back!
How can we differentiate STEMI from Benign Early Repolarization?
Other that just eyeballing it – which I suggest you don’t do. There is a validated calculator that has been developed to help make the differentiation, and it is on MDCalc.
You need to first sure the EKG shows ≥1 mm ST elevation in ≥1 of the precordial leads V2-V4. If it shows any one of the following, then it is NOT normal variant, and is very likely to be LAD occlusion and an MI:
- >5 mm ST elevation
- Non-concave ST elevation
- Inferior reciprocal changes
- Anterior ST depression
- Terminal QRS distortion in V2 or V3
- Q waves in any of V2 to V4
- Any T wave inversion from V2 to V6
The score asks you to then calculate the following:
- Bazett-corrected QT interval in msec
- QRS amplitude in lead V2 in mm
- R wave amplitude in lead V4 in mm
- ST segment elevation 60 ms after the J point in lead V3
A score ≥18.2 is likely to be anterior STEMI (83.3% sensitivity, 87.7% specificity, and 85.9% diagnostic accuracy per the original study from Driver et al.), whereas a score <18.2 is likely to be benign early repolarization.
Now test yourself using this tool on the following case from Dr. Smith’s ECG Blog:
Key Resource
References
Driver BE, Khalil A, Henry T, Kazmi F, Adil A, Smith SW. A new 4-variable formula to differentiate normal variant ST segment elevation in V2-V4 (early repolarization) from subtle left anterior descending coronary occlusion – Adding QRS amplitude of V2 improves the model. J Electrocardiol. 2017;50(5):561-569.
Bozbeyoğlu E, Aslanger E, Yıldırımtürk Ö, et al. A tale of two formulas: Differentiation of subtle anterior MI from benign ST segment elevation. Ann Noninvasive Electrocardiol. 2018;:e12568.
Smith SW, Khalil A, Henry TD, et al. Electrocardiographic differentiation of early repolarization from subtle anterior ST-segment elevation myocardial infarction. Ann Emerg Med. 2012;60(1):45-56.e2.










