If you’ve been following the news then you know that there is an ongoing, and significant infant formula shortage in the United States. The goal of this post is to provide some background and then to offer a summary of the sort of problems that can happen when babies don’t get formula or breast milk.
Why is there an infant formula shortage?
In February there was a contamination issue at an Abbott factory in Michigan that produces most of the Similac formula (Similac, Alimentum, or EleCare), and other brands, for the US. Abbott closed the factory following consumer concerns that contaminated formula (Cronobacter and Salmonella) was linked to two infant deaths. As of the time of this blog post (mid-May) it still isn’t open. Abbott and the FDA have yet to come to an agreement about reopening. This factory shutdown along with all of the supply chain stuff going on (ingredients, packaging, shipping) has lead to the shortage. Per the Wall Street Journal in late April 40% of the most popular Abbott formula brands were out of stock (the normal average is 10% or less). Panic buying has also lead retailers to limit the number of canisters folks can purchase. Still, empty store shelves are rampant. As of mid-May, it’s still not up and running again.
Nearly 20% of babies get formula in the first few days of life. By the time they are three months of age <50% of babies are exclusively breastfeeding.
Nearly one in five babies receive formula within their first two days of life, according to the CDC. By three months, less than half of babies are exclusively breastfeeding, meaning they are taking at least some formula as a supplement. Black, Hispanic, Asian, and American Indian parents are more likely to use formula. Clearly both availability and access to formula are critical issues right now.
Now let’s take a look at some of the things that can happen if parents are diluting formula to stretch it out, using older home recipes, or giving infants alternative sources of nutrition.
Diluting formula to “stretch” out the supply
Parents may elect to add additional water to the formula to give their baby the same volume and to conserve their supplies. This can lead to a number of complications – first, the infant will not get the necessary calories and thus will be at risk of poor growth. More acutely giving extra free water can lead to hyponatremia. Hyponatremia is a serum sodium <135mEq/L. Most children will not be symptomatic when sodium is mildly low – 130-134 mEq/L.
Acute hyponatremia develops in <48 hours – and though this is a little less likely in the above scenario unless the baby is getting pure water – this will lead to severely symptomatic infants. This is most pertinently due to the fact that the brain cannot adapt to the abrupt change in sodium. If the sodium is >125mEq/L the symptoms are less likely to be due to sodium and more to whatever lead them to get to that point (like gastroenteritis). Below 125mEq/L you’ll start to see neurologic symptoms – nausea and malaise are first, followed by obtundation and seizures if the sodium falls below 120 mEq/L. In serious cases brain herniation occurs.
Management of the hyponatremic infant depends on the severity of the sodium deficit and the symptoms witnessed. Patients with acute hyponatremia with neurologic symptoms (seizures) should have immediate replacement of sodium. The seizures won’t stop until you fix the sodium. Management is administration of 3% saline (hypertonic saline) – in aliquots to quickly raise the sodium. One method involves giving 1ml/kg 3% saline every minute until the seizures stop. 1ml/kg will generally raise the serum sodium by 1 mEq/L (how neat). Typically this takes up to 3-4 “doses.”
Chronic hyponatremia develops over days to weeks and is a bit more likely when parents are diluting formula over time. If the symptoms are severe the same hypertonic saline rules apply from above. For milder symptoms you want to aim to correct by 6 to 8 mEq/L/day. If the child is dehydrated and hyponatremic use isotonic saline (NS). You can allow them to eat if they want as long as you are being fastidious about the ins and outs.
Offering cow’s milk before 12 months of age
Remember that it is recommended to give whole milk to toddlers >12 months of age. Under 12 months only breast milk and formula contain enough nutrients. The chief concern that you should be aware of is iron. Additionally 40% of infants on cow’s milk exclusively will have gastrointestinal bleeding. Calcium and casein are also present in higher amounts in cow’s milk. Both of these can lead to reduced iron absorption. The excess calcium is excreted in the urine leading to more concentrated urine. Infant kidneys have lower concentrating ability and thus maintaining water balance is more difficult leading to electrolyte abnormalities and dehydration. Therefore, despite adequate volumes infants fed cow’s milk can still become severely dehydrated.
What about goat’s milk?
The chief problem with goat’s milk is that it does not contain enough vitamin D, vitamin B12, iron and especially folate. folate. This can lead to development of macrocytic anemia (combined folate and iron deficiency usually).
What about soy or almond milk?
Nope – babies should not get either of these. They are deficient in calories and essential nutrients. Commercially available soy milk is generally fortified in calcium and Vitamin D and is thus a little closer to cow’s milk. In generally nut and plant based milks are deficient in calories, protein, calcium, vitamin D and more.
Home formula recipes
Infant formulas are super complex with dense concentrations of protein, fat, vitamins, and minerals – most of which you cannot buy at the grocery store or pharmacy. You can already see how easy it would be to get it wrong. Unfortunately individual recipes are gaining a foothold on social media and being shared by influencers. My advice is not to argue with the families about specific ingredients – instead provide education on why nothing they make at home is likely to meet the needs of their child.
What if a parent can’t find their preferred formula?
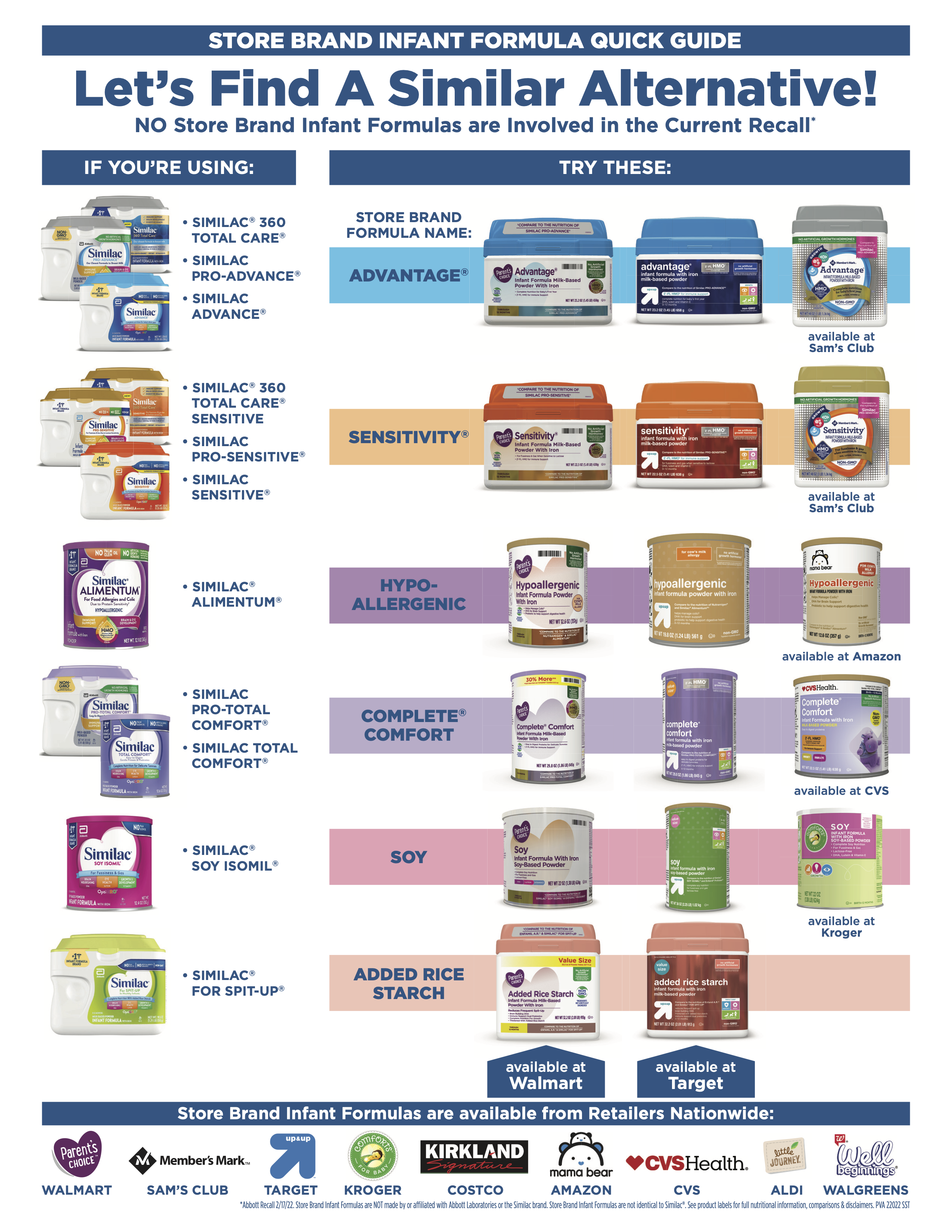
First – NO store brand formulas are involved in the current Abbot recall.
And yes, this is hard. There’s nothing you can do directly to impact the factory or the supply chain. Encourage expectant mothers and parents of newborns to breastfeed and throw all of your expertise and lactation resources at them. Advocate for the families in greatest need and if you have samples in your setting save them for those patients. Tell parents to resist the urge to hoard. And know that brand-name and store-brand formulas are nearly identical and that the same strict standard applied to name-brand formulas apply to generic as well. This goes for most formulas except amino-acid or partially hydrolyzed such as Elecare or Alimentum. In a pinch parents could give a toddler formula for a few days – but they need to be in close contact with their pediatrician about this.
And finally, here is a handy name brand vs generic table to disseminate from StoreBrandFormula.com. You can download the PDF right here:
References
Ziegler EE. Adverse effects of cow’s milk in infants. Nestle Nutr Workshop Ser Pediatr Program. 2007;60:185-199. doi: 10.1159/000106369. PMID: 17664905.
Harrison M, Hilliard R, Lavine E. Case 2: You look like you’ve seen a goat. Paediatr Child Health. 2007;12(5):389-391. doi:10.1093/pch/12.5.389a
Promoting healthy nutrition. In: Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents, 4th ed, Hagan JF, Shaw JS, Duncan PM (Eds), American Academy of Pediatrics, Elk Grove Village, IL 2017. p.167.
FDA Investigation of Cronobacter Infections: Powdered Infant Formula (February 2022). https://www.fda.gov/food/outbreaks-foodborne-illness/fda-investigation-cronobacter-infections-powdered-infant-formula-february-2022 – Accessed 5/13/22
Pisani, Why Is There a Baby-Formula Shortage? What to Know and What’s Being Done About It, Wall Street Journal, 2022 – Why Is There a Baby-Formula Shortage? What to Know and What’s Being Done About It – Accessed 5/13/22












